Don’t Let ‘Perfect’ Be the Enemy of ‘Good Enough’
It’s true: We live in an imperfect world. In the world of ambulatory electrocardiogram (ECG) recording, that’s axiomatic. In a previous issue, we covered the proper way to prepare a patient’s skin for a study. Now we move to the analysis part of the process.
The ECG (heart) signals, which we indirectly measure at the electrodes placed on a patient’s skin, are muscle excitations that propagate through the not-exactly-void chest cavity; through liquids, solids, and layers of tissues of different densities; to the electrodes. Along the way, there is attenuation of an already small electrical signal, the addition of other biological muscle noise as the patient moves around, and, finally, ambient environmental electrical noise — think of the hum you hear on an AM radio when near fluorescent lights. (Does anyone remember AM radio?) In short, the accurate measurement of ambulatory ECG signals is not a trivial problem to solve.
In this noisy, real-world environment, the notion that each and every one of the heart’s roughly 100,000 beats per day can be perfectly categorized is a nearly unattainable goal. However, by the judicious use of the signal processing automation built into our analysis tools and the shrewd eye of a knowledgeable cardiac tech, we can certainly obtain enough credible and correctly categorized data to make reasonable diagnoses.
Core labs often perform studies that do make 100% sure that each and every beat is properly categorized. The cost of these studies is enormous, but the reasons for doing so are critical in the academic and pharmaceutical communities. It is clearly over the top compared to the work required on an everyday basis for most Holter studies.
Use the tools at your disposal to be sure that the beats and strips that are selected as samples in your study are labeled and categorized with 100% accuracy. The key in that statement is “… the beats and strips that are selected …” As a cardiac technician, you have control of that selection. Holter LX Analysis gives you ultimate authority to make those choices, overriding automatic selections and providing the best cases to the cardiologist or physician ultimately responsible for reviewing and making the diagnosis.
The fact that there were some beats that were not able to be categorized because of an artifact (e.g., electrical noise, electrode malfunctions, battery changes, and so on) does not invalidate the importance of the tombstone beat you were able to correctly identify!
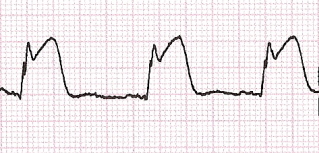
On the other hand, a ventricular premature beat (VPB) incorrectly labeled as a run will not help make your case.

So, in summary, use the tools you have to make the best possible case for what you see. Check carefully that the strips selected and saved to the report are indeed examples of what they are labeled. The overarching philosophy that NEMon builds into its products is that the technician (a human being), not the computer, always has the final say. And that’s exactly as it should be! (See 2001: A Space Odyssey for confirmation!)
[cta]Have new features that you’d like to see in our Holter LX Analysis software? Contact us by email at info@nemon.com, or call us toll-free at 866-346-5837, option 2 (U.S. and Canada), or 978-461-3992.[/cta]

